This Keto Diet Cheat Sheet will help you quickly figure out the basic staple foods of the Keto diet. Even if you’ve done Keto for a while, a quick reference guide is always a good tool to have on hand. Are you new to Keto? You probably have a lot of questions. I know I did when I started out. Can I eat this? Can I eat that? Everything on this list is 100% Keto … [Read more...] about Keto Diet Cheat Sheet – 100% Keto Approved!
The Importance of Speech Therapy to Home Health Care
May is Better Speech and Hearing Month, and Amedisys is proud to celebrate the incredible speech therapists who contribute to our tradition of excellent, clinically distinct care in the home. By preventing, assessing, diagnosing and treating speech disorders—including language, communication, cognitive and swallowing disorders, speech therapy is an essential component to the … [Read more...] about The Importance of Speech Therapy to Home Health Care
From Sonographer to Ultrasound Practitioner: My Career Journey
I have been a sonographer for 18 years, and this year I was awarded Distinguished Sonographer at the 2018 AIUM Annual Convention. I can say without reservation that it is the biggest career honor that I have ever received and a moment that I will never forget. My path to becoming an Ultrasound Practitioner with a faculty appointment in the Department of Reproductive Medicine at … [Read more...] about From Sonographer to Ultrasound Practitioner: My Career Journey
Stars Academy Lahore MCAT/MDCAT Fee Structure
Stars Academy Lahore MCAT/MDCAT Fee Structure MDCAT Test Fee Structure #ClassFeeBooksTotal1MDCAT STUDY + TEST SESSION245003500280002LMDCAT SESSION345003500380003MDCAT & NUMS SESSION405003500440004ROYAL LMDCAT SESSION46500350050000 … [Read more...] about Stars Academy Lahore MCAT/MDCAT Fee Structure
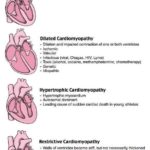
Cardiomyopathy Types Mnemonics Cheat Sheets for Nursing Students
Cardiomyopathy Types Mnemonics Cheat Sheets for Nursing Students #Nursing #Cardiomyopathies dilated cardiomyopathy causes mnemonic The term “cardiomyopathy” refers to “cardio” (heart), “myo” (muscle), “pathy” (disease of). A dilated cardiomyopathy results in left ventricular chamber enlargement, systolic dysfunction and clinical manifestations of congestive heart … [Read more...] about Cardiomyopathy Types Mnemonics Cheat Sheets for Nursing Students